- You are here:
- Home »
- Blog »
- Joint Health / Pain »
- Are My Running Days Over?
Are My Running Days Over?
I started a walk/run program the last week of March. Less than 2 weeks later, my knee began bothering me. It did not start during or after a walk/run but rather happened out-of-the-blue while walking around Carlsbad Caverns.
At first it was just catching, then I noticed popping each time I bent my knee past 90, then I noticed mild pain when squatting or going up stairs. I stopped walk/running and took advil 3x daily. I also began quad strengthening. The pain was gone within a week. I returned to walk/running and found I could run without pain.
I went ahead to an ortho to get an MRI just in case. I figured it was going to be no big deal; instead I find out yesterday that I have grade 2-3 chondromalacia! I am extremely upset and don’t know what to do. My ortho didn’t give me much info. He said the cartilage can’t heal and that PT wouldn’t do me much good. He said I could keep running if it doesn’t hurt and recommended a Synvisc-One shot.
I am very confused because there seem to be literally thousands of opinions on the subject of chondromalacia ranging from “you’ll be fine with a few weeks of PT” to “if you run another step you’ll end up with a knee replacement”. Despite the lack of pain, I have no idea whether to proceed or not. I found your website and noticed you have some different opinions regarding knee issue. I’m not expecting to ever run another marathon. Is is unrealistic to think that I can build up to and maintain 10-15 MPW for fitness? Can this heal? Or are my running days over? Thanks for any advice you can offer.
Barbara (names and places have been changed for privacy)
There’s a lot to unpack in Barbara’s email. I’ll take them one at a time.
#1 – I started a walk/run program the last week of March. Less than 2 weeks later, my knee began bothering me. It did not start during or after a walk/run but rather happened out -of-the-blue while walking around.
A common mistake people make when starting a running program is doing too much, too soon. Usually, the motivator is weight loss or fighting the signs of aging and there’s a sense of urgency around it. So, one day, you decide that you have to do something about this extra weight. You lace up your shoes and off you go.
Weight bearing joints, like the knee and hip for example, respond better to nudging than pushing. Joints that have not experienced the force produced by running (a multiple of bodyweight) are unprepared. The tissue (especially articular cartilage) doesn’t have the internal strength at the cellular level to withstand the pounding. But, cartilage has no nerve or blood supply so it can’t tell you when something is weak or injured. Instead, the surrounding tissue has to do the talking – bone, synovium, tendons, ligaments.
#2 – At first it was just catching, then I noticed popping each time I bent my knee past 90, then I noticed mild pain when squatting or going up stairs. I stopped walk/running and took advil 3x daily. I also began quad strengthening. The pain was gone within a week. I returned to walk/running and found I could run without pain.
The popping, clicking, catching sensations are often created by a reduction in the thickness of the lubricating fluid in the joint (synovial fluid) in response to an inflammatory event. Advil is a non-steroidal anti-inflammatory (NSAID) medication. Quad strengthening (most often in the form of isometrics or “quad sets”) helps to increase the thickness of the fluid. The pain subsided most likely from the reduction in the offending load (stopped running), the use of an NSAID, and the effect of the quad sets.
At this point, the joint is minimally “healthier” even though there’s no pain. It’s inherent strength is the same as when Barbara started running. The next choice, if you must run, which is a discussion unto itself, is to use a graduated running program (and perhaps Barbara did that) – run for a short interval 1-2 minutes, walk for 3 minutes and repeat for 15 minutes of running time for example. And run 2 days a week with several days in between.
#3 – I went ahead to an ortho to get an MRI just in case. I figured it was going to be no big deal; instead I find out yesterday that I have grade 2-3 chondromalacia! I am extremely upset and don’t know what to do. My ortho didn’t give me much info. He said the cartilage can’t heal and that PT wouldn’t do me much good. He said I could keep running if it doesn’t hurt and recommended a Synvisc-One shot.
A lot of people have changes in their joint surface, such as chondromalacia, without any symptoms. Why is that? As long as you stay within the range of forces that your joint can withstand, all is well. When you get too far outside the range, that’s when symptoms appear.
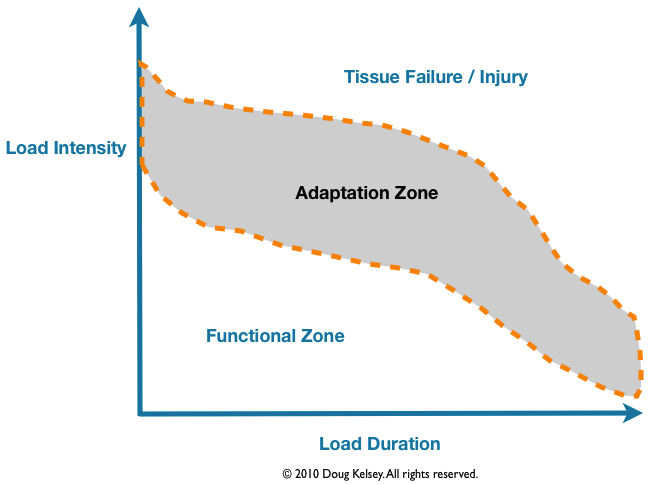
The range we all live in is what I call the “Functional Zone” (FZ). The width of that zone varies by individual and fitness level. What happened with Barbara is that she crossed over into the Tissue Failure / Injury zone and her body was unable to adapt. By resting, taking NSAIDs and performing quad sets, her body moved back down into the Functional Zone where she is asymptomatic.
Injuries, surgeries, invasive procedures leave your joint in a weakened state. This is a difficult thing to comprehend because you might feel just fine but the FZ has shrunk.
A narrower FZ means it’s easier to hurt yourself.
Most physicians will tell you that there’s nothing you can do for a cartilage injury and that’s because that has been their experience. The conventional wisdom is that because cartilage has no direct blood supply, it can’t change or strengthen.
The idea is to strengthen the muscles around the knee to protect the knee but the problem is primarily in the joint not in the muscles. And usually, to reach a level of force that fatigues the muscle, it overloads the joint and your knee ends up stiff, achy or swollen.
It’s true that cartilage has no blood supply and it’s also true that cartilage metabolism is exceptionally low (the rate of energy use). This means it changes slowly. You need great patience and discipline to nudge it back into a healthier state.
Cartilage is, however, mechanosensitive which means it responds to load both in a positive way and in a negative way.
…..human cartilage responds to physiologic loading in a way similar to that exhibited by muscle and bone, and that previously established positive symptomatic effects of exercise in patients with OA may occur in parallel or even be caused by improved cartilage properties.”
Of course, there’s a limit to what your body can do. If you’ve worn off all the cartilage or sections of it leaving exposed bone, your options are limited. Most of the time, you’ll end up in surgery likely with a knee replacement (there is some work promising being done with stem cell therapy though).
#4 – I am very confused because there seem to be literally thousands of opinions on the subject of chondromalacia ranging from “you’ll be fine with a few weeks of PT” to “if you run another step you’ll end up with a knee replacement”. Despite the lack of pain, I have no idea whether to proceed or not. I found your website and noticed you have some different opinions regarding knee issue. I’m not expecting to ever run another marathon. Is is unrealistic to think that I can build up to and maintain 10-15 MPW for fitness? Can this heal? Or are my running days over? Thanks for any advice you can offer.
This is the downside of the Internet. How do you sift through all of the opinions and approaches? It’s a lot of work. I do my best to give my readers and clients the principles and science regarding joint injuries, healing and strengthening. My hope is that this makes the decision process easier.
When we opened our physical therapy practice in the early 1980’s, the common practice following knee surgery, such as Anterior Cruciate Reconstruction, was to place the leg in a cast for a couple of months.
Imagine how stiff your knee would be if you didn’t move it for three months. Rehab was 9-12 months at a minimum.
Surgeons chose to immobilize the joint despite strong evidence to the contrary that moving the joint was much more beneficial to the joint than not moving it as long as you controlled the load. This research was done by Robert Salter, MD. It took decades for it to make its way into everyday practice.
There’s a process you have to follow to get back to a running level and to maintain that level. I don’t know what Barbara has done specifically in her rehab and conditioning nor what she does now.
One thing you don’t want to do is just lace up your shoes and go running. Your joint needs some prep work first, conditioning, and maintenance. I refer to this process as Repair, Rebuild, and Retrain.
One final thought. Why do you run? What are you running toward or from? We do things because there’s a payoff. We gain something from it but we can also hurt ourselves if we’re unaware of our motives.
If you run to manage stress, there are other options. If you run to manage weight, there are other options.
Something to think about.
That’s all I have for now.
Thanks for reading.

PS – If you’re interested in my books, go here.
PPS – If you like this article, why not share it with a friend?
