I’ve run into a small problem.
Like most things in life, nothing goes precisely the way you think it will. In my case, I got off to a good start. I was pleased with my progress, training, everything.
Then, the Texas heat arrived which threw off my training schedule.
I kept training but it wasn’t the plan I had outlined. I couldn’t get outdoors to train on the court so I did the best I could indoors.

Next, I broke my spin bike. A LeMond commercial grade bike. Yeah, I sheared the crank arm right off the thing. I used the spin bike for my speed / interval training.
Strike two.
And then I had to say goodbye to our dog, Abby, who had a brain tumor and other medical issues. I don’t know if any of you have ever had to put your dog or pet down but it’s a very hard thing to go through. Incredibly hard.
Abby was a part of our family for a long time so it really was like losing someone very close to you. I just couldn’t get the image out of my head of her walking down the hallway at the vet’s office and then stopping to turn and look at me as they took her back to an exam room one last time.

I also had some other things going on at the time that distracted me even more.
What happened next is easier to understand in hindsight.
Because I lost the spin bike, to do intervals meant getting over to the gym and adding another hour to my routine and because of the other things happening in my life, my time was tight and I thought the extra time was next to impossible to find (which was not really true if I wanted to do it).
So, I did running intervals.
I’ve done running intervals before but it seems like there’s a speed and duration limit that when I push myself to go past it, I sometimes get hurt.
This time I kept my speed to about 50% of my max and was strict about the duration and frequency and had no problems.
Things were gradually getting back on track.
Until Abby died.
When I need to think or clear my head, I often walk. I get insights, ideas, solve problems while I walk. I don’t know why that is but it happens. Sometimes it’s just “Boom” and problem solved. The combination of the stressors lead to a LOT of walking. Some days I logged 25000 steps or more – about 2-3 times more walking than usual.
And I kept up the running intervals and my training.
You probably know where this is going.
The cumulative load was too much and one day during the rest phase of an interval, I noticed pain on the bottom of my right foot and heel.
The next morning, as my foot hit the floor getting out of bed, I had a sharp, searing pain along the bottom of the foot and into the heel with each step.
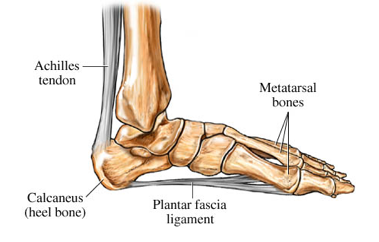
I had a good idea of what this was – a plantar fascial injury – sometimes referred to as plantarfasciitis.
The dastardly plantarfasciitis – a condition that often harasses people for months or years – had come to pay me a visit.
What is Plantarfasciitis?
The suffix “itis” means inflammation. Plantarfasciitis is thought to be an inflammation of the fascia on the bottom of your foot. But outside of the first few days, there are little to no inflammatory cells in the tissue.
Because the “diagnosis” has “itis” in it, physicians and other providers tend to treat the problem with either anti-inflammatories or pain relievers (Advil, Aleve, Motrin or other similar drugs).
Sometimes these things work but for many people, the improvement is short lived. In most cases, when the pain goes away, you feel “healed” and so you resume your life only to find that the injury wasn’t really healed after all but just dormant.
When you chase pain, you can get lost in a hurry. You lose sight of what the real issues is and instead start layering on gimmicks, gadgets and gizmos like Roy McAvoy trying solve his golf swing woes in the movie “Tin Cup”.
Early in my career, when I chased symptoms as fast and as furiously as my clients did, I tried almost as many things to alleviate the symptoms of plantarfasciitis as there are letters in the alphabet : massage, ultrasound, iontophoresis, heel cord stretching, toe stretching, orthotics, taping, positional release, active release, myofascial release, strain-counter strain, strengthening exercises, heel cushions, heel wedges, soft shoes, hard shoes and on and on.
Some of these things seemed to help some people some of the time for a while. But, what I wanted was the same thing my clients wanted: an answer, not a temporary fix.
The problem now is that I’ve sprained the plantar ligament, the soft tissue that runs along the bottom of your foot, and, at its most 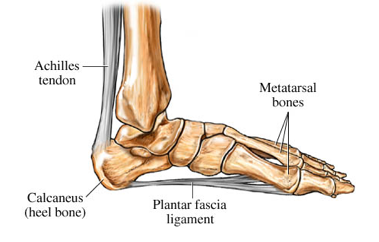 fundamental level, the foot can’t withstand the forces of everyday life. Just walking creates too much physical force on the foot and the result is pain.
fundamental level, the foot can’t withstand the forces of everyday life. Just walking creates too much physical force on the foot and the result is pain.
Healthy plantar fascia has substantial tensile strength – thousands of pounds per square inch. In fact, walking uses less than 50% of the plantar fascia strength so you have plenty of reserve, normally.
But, once you injure the tissue, the strength drops and so does the reserve. The questions become, not “How do I get rid of the pain? How do I make this go away?” but rather “How do I change my body’s ability to withstand force? How do I improve it? How do I get the strength back in my foot?”
Of course, getting the medical profession to use a diagnosis like “plantar ligament sprain” is like asking the Pope to start dating.
Not gonna’ happen.
It would help though to think of this problem as a sprain.
How do you help, for example, an ankle sprain?
Do you stretch an ankle sprain? Rub it? Scrape it with a blunt instrument? Roll it over a lacrosse ball? Load up on drugs?
The answer to solving almost any sprain is something referred to as tissue remodeling or mechanobiology (using an exercise technique I developed years ago referred to as “Target Tissue Training”). The tissues of the body (e.g. bone, cartilage, ligament, or tendon) respond to the stress applied to them. Too much stress, too fast, for too long, and tissues get weaker. Too little stress, too slowly, for too long, and tissues get weaker. Tissues need just the right amount of stress for the right amount of time. When this happens, the tissue adapts and becomes stronger.
The principles of treating an ankle sprain apply to a plantar ligament sprain:
- reduce any additional offending stress – use crutches if necessary.
- protect the tissue from further injury – avoid stretching the injured area, use bracing and taping as needed.
- use pain relievers as needed – this would include both pharmaceuticals and other techniques but recognize that feeling better does not mean you really are better.
- identify a comfortable weight bearing limit – this may mean crutches or other ways to reduce load.
- exercise through three planes of motion within the comfortable weight bearing limit.
- re-test the weight bearing limit and adjust the training.
This is how you rebuild tissue capacity. Everything else is symptom relief – ice massage, strapping, rubbing, poking, physical agents (heat, cold), etc. Not bad or wrong but just keep in mind that what you want is a stronger foot; not one that just feels better.
Things happen (or is that sh*t happens?). How I choose to deal with an unplanned and unpleasant turn of events is to first whine about it, bitch about it (of course internally 🙂 and this stage can last a few hours to months – just being honest) – then start thinking about how to move forward, what can I learn, what it all means and get my butt back in the saddle.
Injuries are most often an invitation to learn something about yourself.
Coming up in a future post, I’ll explain how I’m treating my plantar ligament sprain – using a the principles above but in an unconventional and simple way – that will maybe help you or someone you know.
Stay tuned.